CA OMFS Reimbursement Reductions
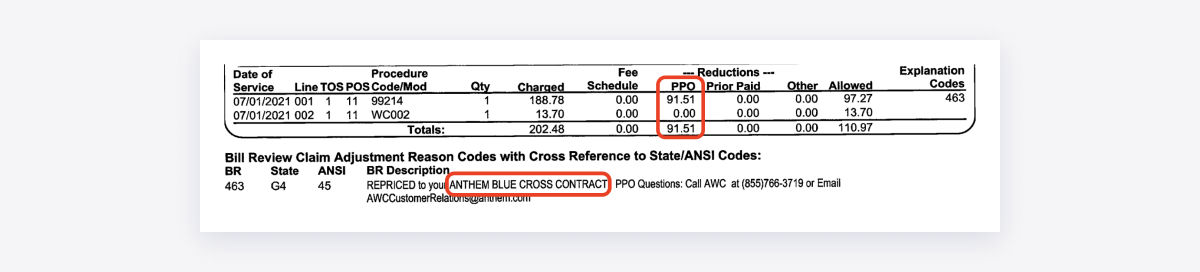
California’s Official Medical Fee Schedule (OMFS) establishes reimbursement rates for medical treatment furnished to injured workers. However, Preferred Provider Organizations (PPOs) and other discount contracting entities can drastically reduce provider reimbursements to well below OMFS rates.
To pressure a provider into signing a discount reimbursement contract, Medical Provider Networks (MPNs) can threaten to exclude a provider from the MPN, if the provider refuses to accept PPO or other network discounts.
Once the provider signs the discount contract, the PPO often quietly sells or leases the discounted rates to other PPO entities, and to the many bill review vendors hired by payers. These bill review vendors then use the discount contract to reduce the provider's reimbursements for countless payers, even those not affiliated with the MPN.
As a result, payers all too frequently issue Explanations of Review (EOR) that indicate the application of a discount contract leased or purchased by the bill review — a contract the provider never actually signed.
These discounts are a revenue management nightmare for providers.
CA OMFS Reimbursement Reductions
In California, when a provider submits a workers’ comp bill electronically, state regulations require the claims administrator to electronically send the provider an EOR disclosing payment information as required by the California Division of Workers’ Comp (DWC).
Below, daisyBill compiles the EOR data that claims administrators electronically send to daisyBill providers. This data represents:
Bills for dates of service on or after Jan 1, 2022
Each procedure for which the payer returned a compliant electronic EOR
Note that the data does not include procedures where the payer entirely denied payment for the procedure ($0 reimbursement).
daisyBill updates this data daily.
CA OMFS Reimbursement Reductions
Health Care Providers
For each daisyBill provider, this data summary calculates the total balance due per OMFS rates, based on the reimbursement amounts the payers actually remitted.
Services Rendered
For each procedure code, this data summary calculates the total balance due per OMFS rates, based on the reimbursement amounts the payers actually remitted.
Fee Schedules
The California Official Medical Fee Schedule (OMFS) consists of 7 separate fee schedules. daisyBill providers submit bills for 5 of these fee schedules (daisyBill does not support bills for inpatient hospital and ambulance services).
daisyBill Reimbursement Data Explained
The data reported on this webpage is for all dates of service on or after January 1, 2022, where the payer remitted a compliant electronic EOR ($0 reimbursements are excluded from data).